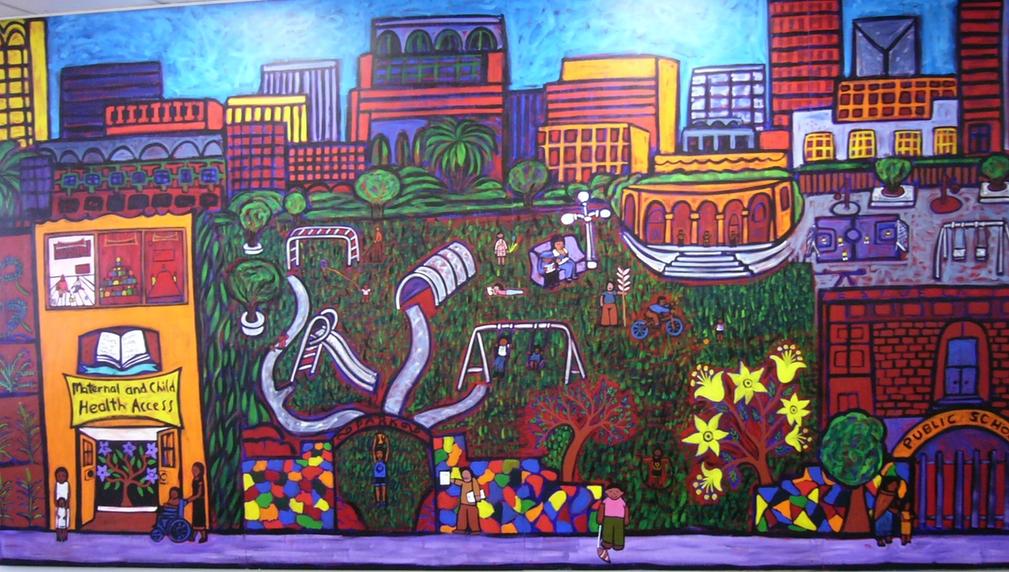
Drowning in Medical Debt? We Can Help!
Medical Debt - applied legitimately or mistakenly - has skyrocketed in California and nationwide. This project would assist with wiping out medical debt as well as assisting those whose type of work may make it difficult to prove income for health coverage applications - who don't get standard paychecks or whose income fluctuates or in other ways don't "fit the mold" and who may give up on health coverage in frustration. MCHA are experts in health coverage and can help make health coverage possible for the most difficult of situations.
What is the primary issue area that your application will impact?
Health care access
In what stage of innovation is this project, program, or initiative?
Expand existing project, program, or initiative (expanding and continuing ongoing, successful work)
What is your understanding of the issue that you are seeking to address?
Medical debt is a huge problem. MCHA gets 1-2 calls a day from people charged after receiving medical care. Insurance may be lacking, insufficient or ignored by the hospital or provider and 2/3 of medical debts are from one-time or short-term medical expense from an acute medical need. People may leave the ER without a bill or receive it later or when they are in collections. Billing practices are confusing, especially for people who don’t speak English or have low literacy. Unpaid accounts go to third-party collections. They have little access to records, making it difficult to know if medical debts are accurate. Medical debt ruins credit. In 2022, $88 billion of medical bills were in collections – affecting 1 in 5 in the US. (Consumer Finance Protection Bureau). LA County’s Board of Supervisors just covered debt for 150,000 residents, leaving some 650,000 struggling with debt (CA Healthline 6-25-24). MCHA wants insurance companies to be responsible for their eligible patients.
Describe the project, program, or initiative this grant will support to address the issue.
Maternal and Child Health Access (MCHA) has assisted low/working-income residents with health coverage enrollment and navigation since 1996. Although “maternal and child” is our name, we assist everyone, from “cradle to grave”. This project would provide support to those with medical debt, but also comprehensively to their family members and others who need to enroll or renew their health coverage, or need help with managed care. MCHA is a social service agency; we offer assistance with utility bills, diapers and baby supplies, a literacy program, classes, CalFresh (food stamps), extra food, and other resources. MCHA will help clients through our phone line, numerous partner agency and coalition referrals, in-reach in our direct service programs, community street outreach and at health fairs and events, and at County General Hospital, at our satellite office. The caller will be assigned an MCHA Health Coverage Navigator, who will assist with researching the bills, determine whether the person is or would be eligible for health coverage (Medi-Cal can cover 3 months retroactively), whether hospital charity programs exist or could be utilized, or any other solution. Of the dozens of cases we assist, very few have actually owed the bill and for those, we’ve been able sometimes to reduce the amount to the Medi-Cal rate, not what the provider requests. As part of the process, MCHA will ask about other needs and other people in the family who may be helped by our assistance.
Describe how Los Angeles County will be different if your work is successful.
If our work is successful, the number of Angelinos with medical debt will decrease and they will have more peace of mind, better credit reports and more purchasing power without discrimination on the basis of their credit.
Our work will add to the Medical Debt coalition which produced the report below, Medical Debt in LA County, http://publichealth.lacounty.gov/chie/reports/Medical_Debt_Report_English.pdf and to the LA County Board’s efforts as defined in their motion. We’d like to be sure that our own county hospitals are not disproportionately adding to medical debt, as in New York, where over 80% of 2023 medical debt lawsuits against consumers were from state hospitals. We’d like to change billing practices and for insurance coverage to be explored before billing a patient. Facilities should know of agencies that help patients, if providers won’t assist. MCHA would suggest that facilities and providers are made aware of organizations that help enroll and ensure coverage.
What evidence do you have that this project, program, or initiative is or will be successful, and how will you define and measure success?
Our project focuses on one aspect of our successful health coverage that is growing and needs direct assistance. As noted, we are able to resolve a majority of the cases of bills people receive/medical debt. We would seek to integrate our work into the Board’s efforts and LA County funding and our overall funding streams for health navigation. We will define and measure success by:
- Purposely integrating our work with the Board of Supervisors’ efforts and encouraging referrals from their offices and elsewhere for incorrect billing and medical debt: We will address a minimum 25% more cases
- MCHA will resolve a minimum of 75% of the cases of debt owed, most situations will have complete debt removal.
- MCHA will contribute policy changes with the Medical Debt Coalition and their report recommendations to help make changes in facilities, reporting, debt collection and how medical debt affects credit
- MCHA will contribute testimonials, stories for news, briefs and other publications.
Approximately how many people will be impacted by this project, program, or initiative?
Direct Impact: 1,500.0
Indirect Impact: 1,000,000.0